The Canary in the Coal Mine -or- How to Improve Kidney Function
By Dr. Douglas Lobay, BSc., ND
Improving kidney function can be difficult and exasperating. As a practicing naturopathic physician, I am always interested in improving the health of my patients. True to the tenets of do no harm, treat the whole patient, and stress preventative medicine, I am looking for ways to improve kidney function in my patients. I have become particularly interested in variations of creatinine and glomerular filtration rate and declining levels of function at the stage 2 and stage 3 kidney disease. I have been fortunate to practice chelation therapy, and I have monitored kidney function in hundreds of patients. Over the years I have analyzed many blood chemistry panels and performed countless urinalyses in the office. I have evaluated kidney function based on serum creatinine levels and estimated glomerular filtration rate (eGFR). Through continuity of care I have compared lab values over time for many patients and tried to figure out what improves kidney function and what causes its decline. Like the canary in the coal that is sent down into mine shafts to sniff out toxins before the miners are sent in, finding ways to improve kidney function before irreversible kidney damage occurs can be indemnifying.
I found Dr. Jenna C. Henderson’s article in the June 2019 Townsend Letter, titled “Is This Actually Kidney Disease, and What Can Be Done About It?” Here is a summary of important points that I learned from this article. Glomerular filtration rate (GFR) is an estimate of kidney filtration. It is associated with serum creatinine levels and also age, gender, and race. It is underestimated in the very young and the very old. If eGFR is decreased, then the first question to be asked is how well hydrated is the patient? Then the next question to be asked is does the patient have high blood pressure or hypertension? Serum creatinine levels can be increased with an increase in muscle mass. Blood urea nitrogen of BUN is a nitrogenous waste product that correlates with dietary protein intake. Renal anemia is due to decreased erythropoietin levels. Potassium levels may be increased with a decreased eGFR. The normal level of urinary pH is between 5.5 and 6.5. There are approximately one million nephrons in the kidneys of the adult human. You lose about 1% of nephrons per year with aging. Blood tests can detect serum creatinine levels, which can be used to estimate glomerular filtration rate. An increase in serum creatinine is associated with a decrease in GFR. Hyperfiltration of the glomerulus is associated with chronic kidney disease. Recovery from a decreased GFR and chronic kidney disease can be limited due to fibrosis of kidney tissue. Active cell division can promote kidney recovery.
Dr. Henderson further describes kidney supplements that may be beneficial for urinary tract infections or UTI’s, kidney stones, and chronic kidney disease. She likes animal studies that use the 5/6 nephrectomy model, in which 5/6 of the kidney is removed. The effect of a treatment can be measured in the remaining 1/6 of the functioning kidney. Dr. Henderson describes the kidney friendly diet. She also suggests the use of dietary supplements that have been shown in some studies to improve kidney function. Some of the supplements mentioned in this article include Epimedium sagittatum, resveratrol, hibiscus, Salvia miltiorrhiza, ubiquinol, citrus bioflavonoids, curcumin (especially tetrahydrocurcumin), and medicinal mushrooms like cordyceps. These supplements can help to ameliorate oxidative stress, inflammation, proteinuria and progressive renal damage.
I am not a kidney specialist, but I have an extraordinary appreciation of the nurses and doctors who work in kidney dialysis units. However, I am interested in how to improve kidney function in early kidney decline such as with stage 2 and 3 kidney disease on an outpatient basis. Stage 2 kidney disease is defined as an eGFR between 60 to 89 milliliters per minute, and stage 3 kidney disease is defined as an eGFR between 30 and 59 milliliters per minute. I decided to do a literature search on PubMed about natural ways to improve kidney function. I discovered that a good place to begin in understanding kidney disease is a thorough review of basic renal physiology.
Kidney Physiology Review
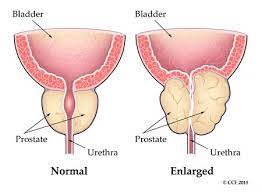
The kidneys are a pair of bean-shaped organs that are normally found in the right and left of retroperitoneal space in the abdomen. The average size of the right kidney is 10.9 centimeters in length and 11.2 centimeters for the left kidney. The average female kidney weighs 115 to 155 grams while the average male kidney weights 125 to 175 grams. Each kidney is supplied by one renal artery and one renal vein. The main function of the kidney is to filter the blood, maintain serum osmolarity, maintain electrolyte and acid/based balance, and remove toxins from the blood. The four mechanisms by which the kidneys work are filtration, re-absorption, secretion and excretion.
The functional unit of the kidney is the nephron. Each kidney has about one million nephrons. Hydrogen, ammonia, potassium, and uric acid are excreted from the nephrons; and water, sodium, bicarbonate, glucose, and amino acids are reabsorbed. Vitamin D or calcitriol is produced in the kidney, and hormones erythropoietin and rennin are also produced there. Each kidney is divided into an outer cortex and an inner medulla. Nephrons, primarily the glomeruli are located in the renal cortex. The afferent arteriole supplying prerenal blood enters the bulbous capsule of the nephron called Bowman’s capsule. The conglomeration of afferent arterioles inside Bowman’s capsule is called the glomerulus. The increased hydrostatic pressure of the afferent arteriole forces blood at high pressure into the glomerulus. Due to the hydrostatic pressure and membrane permeability, low weight molecular molecules are filtered across the capsular membrane. The blood is also filtered across endothelial cells of the arteriole, the basement membrane, podocytes, and around mesangial cells. An amazing one-fifth of the entire human blood supply is filtered each minute. An incredible amount of 180 liters of filtrate is produced each day through the renal glomerulus. The efferent arteriole leaves Bowman’s capsule with the remaining filtered blood. Meanwhile, the filtrate produced across the glomerulus drains down across a series of tubules, namely the descending proximal tubules, loop of Henle, the ascending tubules and the distal convoluted tubules and collecting ducts. The early proximal tubule reabsorbs glucose, amino acids, sodium, chloride, phosphate and water. The loop of Henle is a u-shaped bend of tubules that includes the thin descending loop and a thicker ascending loop. The thin descending loop of Henle reabsorbs mainly water that leads to concentration of urine produced. The thick ascending loop of Henle reabsorbs electrolytes including mainly sodium, 3 potassium chloride, magnesium, and calcium. The distal convoluted tubules reabsorb mainly sodium and chloride and the collecting ducts also reabsorb sodium and water. The urine filtrate produced leaves the collecting tubules through the renal medulla and ultimately through the calyces to the ureters and bladder.
Creatinine is a breakdown product of creatine phosphate found in muscles and is usually produced at a fairly constant rate and is somewhat dependent on muscle mass. About 1% to 2% of muscle creatine is converted to creatinine on a daily basis. It is a nitrogenous compound removed by the body primarily through glomerular filtration and a small amount through the proximal tubules. Men, through increased muscle mass, have higher creatinine levels than females. Serum creatinine levels are 0.5 to 1.0 milligrams/deciliter or 45 to 90 micromoles/liter in females and 0.7 to 1.2 milligrams/deciliter or 60 to 110 micromoles/liter in males. Lab values of creatinine also vary slightly from lab to lab. Creatinine has also demonstrated antibacterial and immunosuppressive properties. Creatinine levels can also be increased with high protein dietary consumption. Creatine clearance is associated with glomerular filtration rate. False elevations in serum creatinine can occur. Factors that can increase serum creatinine include race, age, body size, gender, menstruation, diurnal variation, intense exercise, and increased protein intake. Approximately 15% of creatinine is secreted by the renal tubules. Certain drugs can increase serum creatinine. These drugs include Trimethoprim, cimetidine, and H2 blockers. Rhadmyolysis or acute muscle damage can also increase creatinine levels.
Urea is a nitrogenous by byproduct of muscle metabolism produced in the urea cycle by conversion of nitrogen from amino acids to ammonia compounds. BUN production is somewhat more variable than creatinine and less reliable as an indicator of kidney filtration. Urea is increased from a diet rich in protein. The BUN to creatinine ratio provides some interesting information about the possible location of kidney dysfunction. A BUN to creatinine ratio greater than 20:1 indicates a prerenal cause. A BUN to creatinine ration between 10-20:1 indicates a post-renal cause. And a BUN to creatinine ratio of less than 10:1 indicates an intra-renal cause.
Glomerular filtration is an estimate of kidney function and degree of kidney disease. Glomerular filtration or GFR represents the flow of plasma into Bowman’s space in a specific period of time. Kidneys receive 20 to 25% of blood volume cardiac output equaling 1.0 to 1.2 liters per minute. Glomerular filtration rate is correlated with serum creatinine levels, age, body size, race, and gender. Stage 1 kidney disease has a GFR greater than 90 ml/minute and indicates normal kidney function. Stage 2 kidney disease has a GFR between 60 to 89 ml/minute indicates mild loss of kidney function. Stage 3a kidney disease has a GFR between 45 to 59 ml/min and indicates a mild to moderate loss of kidney function. Stage 3b kidney disease has a GFR between 30 to 44 ml/minute and indicates moderate to severe loss of kidney function. Stage 4 kidney disease has a GFR between 15 to 29 ml/minute and indicates severe loss of kidney function. Stage 5 kidney disease has a GFR less than 15 ml/minute and indicates severe kidney failure. Many labs use an arbitrary level of GFR less than 60 ml/minute to indicate kidney disease. Also the degree of protein or albumin in the urine has been correlated with the degree of loss of kidney function.
Hormones affect reabsorption of different molecules in the kidneys. Anti-diuretic hormone or ADH, produced in the posterior pituitary gland in the brain, is also known as vasopressin and stimulates water reabsorption through the kidney tubules. Vasopressin goes to the distal and collecting tubules and promotes the reabsorption of water back into circulation. A low blood pressure can stimulate the release of vasopressin into systemic circulation. Copeptin derived from the c-terminal is a surrogate marker of vasopressin and is more stable and measurable than ADH. Aldosterone produced in the adrenal glands stimulates sodium reabsorption through the kidney tubules. Parathyroid hormone, produced in the parathyroid glands, alters phosphate and calcium reabsorption.
Chronic kidney disease or CKD affects about 10 to 15% of the adult population of Western countries. It is a major risk factor for cardiovascular disease and death. CKD has been associated with hypertension, diabetes, and atherosclerosis. Structural and functional abnormalities of renal tissue show up in just three months after declining kidney function. There can be a genetic component to kidney pathology and kidney disease. Kidney disease can be further divided depending on the deposition of immune globulins. Proliferative kidney disease is an immune-dependent pathological process that results in inflammation and the deposition of immune complexes in the glomerulus and tubules. Non-proliferative kidney disease is not caused by immune globulin deposition and is not immune dependent. The podocyte of the glomerulus plays a central role in kidney disease pathology. Immune complexes can be deposited in mesangial cells of the glomerulus.
Chronic kidney disease is associated with renal fibrogenesis causing glomerular sclerosis and tubular interstitial fibrosis. Fibrogenesis induces inflammatory changes in the glomerulus and tubules. Inflammatory filtrate, profibrotic cytokines, and fibroblast proliferation occurs. Tubulo-interstitial inflammatory infiltrates include proteinuria, immune deposits, chemokines, calcium phosphate, metabolic acids, including uric acids and oxidized lipids. The net effect is that these deposits further caused renal deterioration.
Non-steroidal anti-inflammatory drugs decrease kidney prostaglandins. A decrease in prostaglandin synthesis, which regulates vasodilation at the glomerular level, causes a decrease in renal blood flow. This disrupts compensatory vasodilation causing renal vasculature constriction. NSAIDS also cause increased pressure in the renal interstitium for up to one week after starting these drugs. About 15% of acute kidney injury is due to NSAID consumption.
Diet and Kidneys
There is a direct association between water intake and kidney function. Water intake is related to chronic kidney disease, polycystic kidney disease, and nephrolithiasis or kidney stones. Benefits have been noticed when urine output has been measured to be between 3 to 4 liters per day. Increased water intake blocks the renal vasopressin V2 receptor. A comprehensive literature review studied the effects of hydration on kidney function. Increased water intake decreases vasopressin levels. Hydration can improve kidney function in all forms of chronic kidney disease, recurrent renal calculi, and slow renal cyst formation.2 A beneficial effect on kidney function in patients who are at risk for development of chronic kidney disease was noted. Although increased hydration and reduced vasopressin secretion appear to slow progression in patients with chronic kidney disease, over-hydration can be detrimental in patients with end-stage kidney disease. Beneficial effects have been noted in patients with earlier chronic kidney disease, diabetic nephropathy, and nephrolitiasis.
A randomized controlled trial was conducted for one-year duration to study the effect of increased water intake on kidney function. Increased water intake was associated with a decreased concentration of calcium oxalate, calcium phosphate, and uric acid. Increased urine output between 2 to 2.5 liters per days was a consequence of increased water intake. Increased water intake was associated with a decreased growth rate of polycystic kidneys. Six hundred and thirty-one participants with stage 3 chronic kidney disease and a GFR between 30 to 60 ml/minute were selected for this study. The participants were coached to increase water intake by 1.0 to 1.5 liters per day (4 to 6 cups of water in addition to other beverages usually consumed). Plasma copeptin levels were directly correlated with anti-diuretic hormone or vasopressin levels. Vasopressin was the first hormone released during the early stages of dehydration. The increased level of vasopressin was correlated with early kidney disease. Other surrogate markers, including estimated glomerular filtration rate, copeptin, and microalbuminuria, were measured. Increased water intake was associated with improved kidney function markers.
Fluid self-management recommendations were made for prevention of kidney stones based on epidemiological evidence. A urine fluid output of 2.5 liters per day or more was recommended. Potassium-rich foods protected against kidney stone formation. Increasing fluid intake of 500 ml of water per day decreased kidney stone formation. Tea and alcohol consumption also decreased kidney stone formation. Fruit juice, soda and pop did not decrease kidney stone formation and were suggested to increase rates. Coffee and milk showed inconsistent results and could not be recommended as a fluid to decrease kidney stone formation. The combined interaction of environmental exposure, dietary habits, and genetic factors cause kidney stones. Water intake is recommended to be three liters or greater per day to help prevent kidney stones. It is not the quality of water, rather the quantity of water consumed that matters in most cases. The correlation between water hardness, which increased mineral concentration, and the development of kidney stones remains controversial.
Low-protein and plant-based diets are beneficial in chronic kidney disease. Low protein diets can reduce protein intake, phosphorus and sodium. Plant-based diets are low in saturated fats, high in fiber, and high in unsaturated fats and potassium. These diets are low in creatine.
High salt intake can have detrimental effects on kidneys by affecting glomerular function. Increased glomerular hyper-filtration, increased filtrate formation, and increased glomerular pressure are a consequence of high-salt consumption. Increased sodium intake blunts the anti-proteinuria effects of various drugs, including ACE inhibitors. Increased sodium further causes increased blood pressure, increased renal hypertrophy, renal fibrosis, decreased glomerular basement membrane, and decreased anionic membrane function. Restricting sodium intake is an important preventable measure in patients with chronic kidney disease.8
A modest coffee intake of one to two cups per day decreased the risk of developing chronic kidney disease. The odds ratio of developing kidney disease was 0.76 with drinking one cup of coffee per day. The odds ratio of developing kidney disease was 0.80 by drinking two cups of coffee per day.9Decreased plasma creatinine levels were observed in mice that consumed decaf coffee for two weeks. High-dose decaf coffee increased nucleotide activation in the kidney cortex, which increased kidney function. Meta-analysis of four observational studies with 14,098 people showed no significant association between coffee intake and development of chronic kidney disease. Interestingly however, the odds ratio was 0.81 in females and 1.10 in males.
Green tea consumption was associated with a decreased risk of developing kidney stones in a large prospective study of elderly Chinese people. The odds ratio was 0.78 in males and 0.80 in females.1 Green tea polyphenols protected the kidneys against oxidative stress damage in early renal damage.
Apple cider vinegar induces a protective effect on oxidative damage to the kidney in ovariectomized mice fed a high-cholesterol diet.
Dietary treatment of urinary risk factors for renal stone formation was assessed. A general conservative therapy was recommended. Decreased fluid intake was associated with decreased urine output less than 2 liters per day. Dietary calcium supplementation was not recommended. Dietary calcium less than 1 gram per day, low protein diet, and low sodium diet were recommended. Mild dietary salt intake was associated with decreased calcium excretion. Calcium supplementation was recommended between 800-1200 mg per day. A low normal protein diet was associated with decreased calcium loss. Alkaline citrate minerals were recommended. Increased fruit and vegetables excluding high oxalate food were suggested. Increased consumption of citrate foods and melons increased urinary citrate levels.
Vitamins, Minerals, and Kidneys
Oxidative stress is a disruption of the balance between the production of reactive oxygen species or ROS and antioxidant defense mechanisms. Oxidative stress was identified in early kidney disease. Suggested potential useful antioxidants have been identified in food and supplements. Some proposed antioxidant supplements include vitamin B, C, D and E, coenzyme Q10, L-carnitine, alpha lipoic acid, curcumin, green tea, flavonoids, polyphenols, omega-3 polyunsaturated fatty acids, statins, trace elements and n-acetyl cysteine.16
In a double-blind randomized controlled trial, 60 patients with diabetic nephropathy were supplemented with 1200 IU of vitamin E or placebo for 12 weeks. Vitamin E supplementation was observed to increase serum levels. Decreased protein to creatinine ratio, decreased tumor necrosis factor or TNF, decreased matrix metalloproteins, and decreased malondialdehyde levels were noted. No effects on other biomarkers of kidney disease were observed. Decreased levels of inflammation, kidney injury, and oxidative were also observed.17 Vitamin E supplementation of 300 milligrams per day for 12 weeks with 20 diabetic and 20 non-diabetic patients with end stage kidney disease undergoing hemodialysis. Vitamin E supplementation improved HDL levels and vascular endothelial function.18
High homocysteine has been correlated with kidney disease. Low levels of vitamins B12, B9, and B6 have been associated with high homocysteine levels. One hundred and forty-eight 7 patients with chronic kidney disease from the Ukraine were measured for homocysteine levels; 58.7% of patients had high homocysteine levels. Homocysteine was believed to be a specific indicator of low vitamin status, especially for vitamin B9 or folic acid.19
Recurrent kidney stone formation in patients with normal renal function who have a defect in ascorbic acid to oxalate metabolites should restrict vitamin C supplementation to less than 100 mg per day. However, a large-scale prospective study showed that the group with the highest quintile of vitamin C intake, which was greater than 1500 mg/day, had the lowest risk of kidney stone formation.
Long-term intake of vitamin D resulted in an increased risk of hypercalcemia and hypercalciuria, which appeared to be not dose related. However, vitamin D supplementation did not increase the risk of kidney stone formation. It was recommended that large randomized controlled trials of vitamin D are needed to confirm these findings.
Magnesium is utilized for over 300 different biochemical reactions in the human body. Magnesium helps to decrease vascular calcium and decrease phosphate absorption.
Supplements and Kidneys
Coenzyme Q10 is a strong antioxidant and mitochondrial nutrient. Decreased Q10 levels have been observed in patients with chronic kidney disease. A meta-analysis of seven randomized controlled trials of patients with chronic kidney disease were selected from 721 potential papers from PubMed, Cochrane, and other medical databases were selected. Coenzyme Q10 supplementation was associated with decreased total cholesterol, decreased LDL cholesterol, decreased malondialdehyde, and decreased creatinine levels. Triglyceride levels as well as HDL cholesterol, glucose, insulin and CRP levels were not affected by Q10 supplementation.24 The effect of coenzyme Q10 supplementation was studied on 72 rats exposed to radiation-induced nephropathy. Q10 was administered at a dose of 10 mg/kg body weight. Signs of poor kidney function were observed after radiation exposure. Q10 supplementation decreased BUN and creatinine levels. Q10 seemed to attenuate glomerular and tubular function in irradiated kidneys. Administration of Q10 seemed to alleviate radiation induced kidney damage.25 The effect of benfotiamine, a derivative of vitamin B1 or thiamine and co-enzyme Q10 was studied a group of rats that had gentamycin-induced kidney damage. Gentamycin was severely toxic to rats. Benfotiamine supplementation decreased nephrotoxicity, decreased BUN and creatinine levels and decreased malondialdehyde levels. Q10 supplementation decreased necrotic tubular tissue levels and hyaline accumulation.
Resveratrol is a natural polyphenolic compound found in grapes and other compounds. Resveratrol is a robust antioxidant that scavenges reactive oxygen species or ROS. Resveratrol is also a SIRT-1 activator, which increases enzyme functions, decreases apoptosis, and increases mitochondrial biogenesis. Resveratrol has demonstrated to have some renal protective effects.
N-acetyl cysteine or NAC administration ameliorates renal function by decreasing oxidative damage as observed in Wistar rats with induced kidney damage following bilateral ureteral obstruction.
Acetyl-l-carnitine improved energy metabolism in the kidneys of hypoxic-ischemic brain-injured rats.
L-carnitine levels have been observed to be low in patients with advanced kidney disease. A systematic review of the evidence of carnitine and kidney disease was undertaken. Fourteen references were identified for review. A meta-analysis shows some useful pieces of information and the potential benefit of carnitine supplementation in patients with advanced kidney disease. The authors recommend carrying out better designed studies to show the potential benefits of this supplement.
Lipoic acid is a free radical scavenger of reactive oxygen species (ROS) and nitric oxide (NO). It’s mechanism of action is not completely understood but is believed to operate with different kinase pathways. Lipoic acid is known to affect multiple signaling pathways and has demonstrated renal protective effects in contrast-induced kidney injury.
Melatonin prevents drug-induced renal injury by decreasing inflammatory cytokine production and decreased aquaporin water channels in male rat’s kidneys with bilateral ureteral obstruction.32
Herbs and Kidneys
Berberine showed antioxidant, anti-apoptotic, and anti-inflammatory activity in diabetic rats exposed to nephrotoxic streptozotocin. Decreased levels of BUN and creatinine were observed with berberine doses of 100 and 150 milligrams per kilogram. Improved histopathological kidney function was also observed with declining levels of BUN and creatinine. Increased free fatty acids and disturbed mitochondrial function play a role in diabetic kidney disease. Diabetic mice were fed berberine for eight weeks. Berberine reversed glucose and lipid metabolic podocyte damage, basement membrane thickening, mesangial expansion and glomerular sclerosis. Decreased podocyte apoptosis was also observed.34 Berberine demonstrated a protective effect on kidney and liver function in rats exposed to iron overload for two weeks. Increased iron consumption increased oxidative damage causing histopathological changes to these organs. Elevated levels of oxidative damage also increased malondialdehyde levels, which is a marker of oxidative damage. Berberine protected the liver and kidney against ferrous sulphate-induced toxicity, reduced lipid peroxides, and also chelated iron.35 Chronic diabetic kidney disease causes microvascular damage to the renal glomerulus and causes interstitial fibrosis to the renal tubules. Berberine showed a significant positive effect by decreasing total blood sugar levels, improving renal hemodynamics, improving lipid profiles, and was shown to attenuate local and systemic inflammation.
Berberine protects renal tubular cells from ischemia and reperfusion injury in rats. Berberine protects renal tubular epithelial cells from hypoxia and reperfusion mitochondrial dysfunction by regulating sirtuin-2 and c53 pathways.37 Berberine also protects renal tubular epithelial cells from hypoxia and apoptosis through activation of HIF-1alpha in the signaling pathway suggesting that berberine could be a potential drug in diabetic ketoacidosis.
Hydrangea or Hydrangea paniculata extract was given to mice with cisplatin-induced kidney damage. Improved renal function was observed with decreased creatinine and BUN levels. The coumarin glycosides of this plant were believed to attenuate oxidative stress, decrease tubular injury and decrease apoptosis. Decreased inflammatory cytokines and regulation of protease enzymes, including caspase, an enzyme involved in inflammation and programmed cell death, were noted. Hydrangea extracts ameliorated kidney damage by antioxidant activity and suppressing harmful renal infiltrates and tubular apoptosis. Decreased renal infiltrates down regulated signaling pathways, which further decreased macrophage and neutrophil activation.39
Hydrangea extracts containing coumarin were given to mice with acute septic kidney injury. Bioactive coumarin compounds isolated from Hydrangea paniculata were identified to be umbelliferone and esculetin. Hydrangea demonstrated specific antioxidant and anti-inflammatory activity on kidney tissue. Decreased infiltrate of macrophages and neutrophils in renal infiltrate was noted. Decreased BUN levels and decreased tubular interstitial injury were noted. Improved kidney function and increased animal survival were observed.40 Water extracts of Hydrangea paniculata were rich in coumarin glycosides. A water extract of this plant was given to diabetic rats that were exposed to strepozotocin kidney damage. Hydrangea extracts were given once per day for three months. A decrease in BUN and creatinine was observed. The hydrangea extract upregulated some enzyme activity and decreased other signaling pathways.
Silybin from milk thistle (Silybum marianum) protected against cisplatin-induced acute kidney injury. Silybin increased sirtuin-3 or Sirt-3 expression in mice, which was shown to protect against cisplatin-induced kidney damage by decreasing tubular apoptosis and increasing mitochondrial function. A standardized mixture of silymarin flavonolignans from milk thistle has demonstrated antioxidant activity for reactive oxidant species (ROS). Contrast-induced nephropathy caused tubular injury in mice kidneys. Silymarin preserved renal function by improving glomerular and tubular function in a dose dependent manner in mice exposed to contrast injury.
Apigenin is a flavonoid isolated from celery (Apium graveolens). Apigenin is an anti-hypertensive flavone that is abundant in celery. Apigenin acts as an agonist of transmut receptor-potential vanilloid-4 or TRPV4 in rats. Apigenin has demonstrated promising anti-hypertensive activity in treating hypertensive-induced renal damage in those who consume a high sodium diet.44 A hydroalcoholic extract of celery was used to treat uncomplicated urinary tract infection in mice caused by uropathogenic E.coli. A direct anti-adhesive effect of celery on the urinary epithelium was observed in a dose dependent manner within four to seven days of treatment. The extract significantly reduced the bacterial load in uncomplicated UTIs in this group of mice.45 In another study, rats were exposed to a chlorinated propanediol chemical that induced kidney damage. Apigenin decreased serum creatinine and reduced kidney damage by modulating mitochondria dependent caspase activity.46
An herbal decoction of the Chinese medicine Huangqi-Danshen was fed to a group of rats for four weeks. Improved levels of BUN and creatinine were observed after treatment. Decreased tubular atrophy and decreased interstitial fibrosis was also observed. Also improved mitochondrial function was also observed in kidney tissue of these animals.47 A water extract of 10
Salvia miltiorrhiza called Danshen was studied against renal injury in rats exposed to cadmium. The salvia extract displayed antioxidant activity, decreased swelling of renal tubule epithelial cells, and improved overall renal function.48 Salvia miltiorrhiza extract was given to diabetic rats and was shown to decrease renal injury and damage and improve glycolipid metabolism. Multi-modal effects were observed, including phospholipid, arachidonic acid, wnt/B-catenin and TGY-B signaling inhibition.49 Salvianolic acid A (SAA) is a phenolic carboxylic acid derivative of Salvia miltiorrhiza. SAA helped to decrease inflammation and decrease renal tubular fibrosis in six rats that were exposed to doxorubicin-induced nephrotoxicity. SAA was believed to be a signaling molecule that decreases activation of natural factor beta-kappa (NF-KB) and thereby decreases inflammatory pathways.50
An aqueous extract of parsley (Petroselinum sativum) was studied on a group of rats. The parsley extract showed diuretic effects including decreased sodium reabsorption, decreased potassium secretion, increased potassium concentration in the intercellular space, and decreased potassium efflux across cellular tight junctions. An inhibition of sodium/potassium pump activity was noted leading to a reduction of sodium reabsorption and potassium loss.51 The effects of an aqueous extract of parsley on ethylene glycol-induced kidney calculi in rats were studied. A decrease in calcium oxalate stone formation and deposition were noted.52.
The effect of Diyarbakir watermelon juice on lipid peroxidation was studied in rats after exposure to carbon tetrachloride. The watermelon juice showed antioxidant activity and inhibition of lipid peroxide formation.53 However, excessive watermelon consumption was associated with high potassium levels or hyperkalemia and increased symptom burden of end stage renal disease.54 The anti-urolithiatic and diuretic effects of watermelon (Citrullus lanatus) was studied in a group of male rats. Kidney protective effects and a suppression of calcium oxylate precipitation were noted. Increased creatinine clearance, decreased urea, decreased sodium, and urinary output were also observed. Watermelon pulp displayed significant anti-urolithic and diuretic activity.55
Thirty-four neutered cats were put on a nutraceutical diet containing Lespedeza, Vaccinium and Taraxacum herbs for 90 days. There was a significant decrease in BUN, creatinine in lab samples and a decrease in total protein lost from their kidneys.56 Researchers compared the effects of taraxasterol aqueous extract from dandelion (Taraxacum officinale) aerial parts and potassium citrate on oxylate crystallization in vitro. Taraxasterol and potassium citrate extract decreased calcium oxylate crystallization more than taraxasterol alone. It was hypothesized that there was a synergistic effect between Taraxacum extracts and potassium citrate.57
The effect of green asparagus (Asparagus officinalis) extract was studied in hypertensive rats. A constituent of asparagus, 2’-hydroxynicotianamine, was believed to act as an angiotension converting enzyme or ACE inhibitor. The asparagus extract decreased blood pressure levels and improved renal function.58 The effect of asparagus extract was studied in bisphenol-causing liver and kidney damage in Wistar rats. Coadministration of asparagus extract and bisphenol exposure increased total antioxidant capability and decreased malondialdehyde levels, which is indicator of oxidative stress. Decreased levels of oxidative damage to liver and kidneys with asparagus consumption were noted.59 11
Black seed (Nigella sativa) has been used in the prevention of kidney stones. In a placebo controlled double-blind study 60 patients consumed 500 mg of black seed or placebo twice per day for 12 weeks. Those who consumed black seed were 44.4% more likely to excrete kidney stones compared to 15.3% who took placebo. The black seed-treated group showed a decrease in the size of kidney stones in 51.8% of people while stone size was unchanged in 57.6% of those who took a placebo.60 The effect of black seed oil was studied in cisplatin-induced nephropathy in rats. The group that consumed black seed oil showed a marked decrease in histopathological changes to kidney tissue. Black seed displayed antioxidant activity and was shown to modulate enzyme activity in the kidney.61
The long-term survival rate was studied in retrospective analysis of Taiwan patients with chronic kidney disease who took a Chinese herbal medicine containing Rheum officinale. The Chinese herbal medicine improved long-term survival in patients with CKD suggesting that this medicine is an effective adjuvant in individuals with chronic kidney disease.62
An aqueous extract of hibiscus (Hibiscus sabdariffa) was given to rats for 28 days with adenine-induced kidney disease. The hibiscus extract demonstrated a similar effect to the angiotensin converting enzyme or ACE inhibitor drug lisinopril. The hibiscus extract was further demonstrated to decrease the progression of chronic kidney disease.63
Goldenrod (Solidago virgaurea) has been used for centuries for the treatment of urinary tract disease. Goldenrod has displayed anti-inflammatory, anti-urothiac, diuretic, anti-spasmodic, and analgesic effects. Goldenrod has been used for urinary infections and inflammation, to prevent kidney stone formation, and to remove urinary gravel. It appears to be safe and non-toxic and no adverse side effects were noted.64
Curcumin was reported to have kidney protective effects.65 Four hundred and fourteen patients with chronic kidney disease with a glomerular filtration rate between 15 to 60 ml/min were included in this randomized controlled trial. Patients consumed 90 milligrams of micro-particle curcumin once daily or placebo for six months.
Butein from Chinese lacquer tree (Rhus verniciflua) has been shown to improve kidney function in cisplatin-induced acute renal failure in rats. Butein upregulates aquaporin 2 channels in the kidney cortex and medulla.66
Other herbal medicines have also been suggested to improve kidney function, including beets, chamomile, Chanca Piedra, cinnamon, ginger, gravel root, horsetail, marshmallow, nettles, and uva ursi to name a few.
Toxins and Kidneys
Certain dietary supplements and herbs have been identified to cause potential kidney toxicity and renal damage. Implicated herbs include Chinese yew (Taxus celebica), Callilepsis laureola, morning cypress (Cupressus tunebris), Saint John’s wort (Hypericum perforatum), Thunder God vine (Tripteryglum wildfordi), tribulus (Tribulus terrestris), and wormwood (Artemnesia alba). Herbs no longer sold in the US include chocolate vine (mu tong or Caulis aristolochiae), Guang fang ji (Artistolochia fungchi), and Ma huang (Ephedra sinensis). Other dietary supplements include sheep bile, chlorella, chromium, creatine, fish gall bladder, glucosamine, hydrazine, NO-xplode, Spanish fly, and excessive consumption of vitamins A, C, D and germanium. In descending order of toxicity, the top two offenders were aristolochic acid in the herb Guang fang ji and chocolate vine. Kidney toxic foods include ajenkol bean, gall bladder from carp fish, puffer fish, star fruit, and uncooked yam powder or juice.
Aristolochic acid from Aristolochia species of herbs causes nephropathy. In the 1990s aritstolochia was used in various weight-loss products. Consumption of products containing aristolochic acid causes kidney injury and renal damage. Increased serum creatinine, significant anemia, and histopathological changes in renal interstitial infiltrates causing severe fibrosis occurred.68
Chronic kidney disease is associated with an increased level of uremic toxins. Certain toxins may be modified by the gut microbiota. Potential toxins identified include phosphates, l-carnitine, choline, phosphatidylcholine, tryptophan and tyrosine, tri-methylamine-n-oxide, indoxy sulphate, p-cresyl sulphate, and indole-3 acetic acid.69
Recommendations
It is clear that diet and nutrition plays an important role in kidney function. Water intake can be measured and increased in individuals with stage 2 and 3 chronic kidney disease. There are exceptions to increased water intake especially with people with lung and peripheral edema. Fluid restrictions are further necessary in individuals with advanced kidney disease, including stage 4 and 5 levels. Salt and sodium should be restricted in usually all levels of kidney disease, especially with high dietary intake. Protein intake can be measured and modulated in individuals with high dietary intake. Electrolyte levels, including potassium and phosphorus, can be monitored and measured along with creatinine and GFR in basic lab tests. Recommendations can be made after reviewing lab values. Eating a diet rich in fresh fruits, vegetables, whole grains and cereals and high-quality protein is strongly suggested. Limiting processed foods, highly refined sugar foods, excessive protein and alcohol is also suggested. Eating better can perhaps help kidney function and improve overall health.
A review of the scientific literature suggests that vitamins and minerals, supplements and herbal medicines may help to maintain and, in some cases, improve kidney health. Many of the studies are done on animal models that include rats and mice. While interesting it is important to note that these are not humans. There are some human studies that are interesting and show benefit, but it clear that most of the conclusions are preliminary at best. Further randomized double blind placebo-controlled trials are suggested with larger patient populations and limiting extraneous factors. This is not to say that certain nutrients and supplements are not beneficial and cannot actually improve kidney function. There are many vitamins, minerals, supplements and herbal medicines as discussed in this article that have been shown to prevent kidney decline and may improve renal function. How they combine with other nutrients is not known but probably not harmful in recommended doses. They are certainly worth a try with individuals with declining kidney function, especially earlier in stage 2 and 3 levels of kidney disease. Discussing a treatment plan with a licensed naturopathic physician or other qualified health professional is recommended. Of course, it is caveat emptor or patient trial and error. Like the canary in the coal mine, I think kidney function decline with early kidney disease can be averted with dietary changes and nutritional supplementation.
Dr. Douglas Lobay, BSc, ND
Douglas G. Lobay is a practicing naturopathic physician in Kelowna, British Columbia. Dr. Lobay graduated with a bachelor of science degree from the University of British Columbia in 1987. He then attended Bastyr College of Health Sciences in Seattle, Washington, and graduated with a doctorate of naturopathic medicine in 1991.
While attending Bastyr College, he began researching the scientific information on the use of food, nutrition, and natural healing. Dr. Lobay enjoys research, writing, and teaching others about good health and good nutrition.
He is the author of four books and numerous articles in magazines. He also enjoys hockey, skiing, hiking, tennis, and playing guitar.
References
1. Wang CJ et al. The medicinal use of water in renal disease. Kidney Int. 2013 Jul:84(1): 45-53.
2. Clark WF et al. Hydration and Chronic Kidney Disease Progression; A Critical Review of the Evidence. Am J Nephrol. 2016: 43(4):281-92.
3. Clark WF et al. Hydration and Chronic Kidney Disease Progression: A Critical Review of the evidence. Am J Nephrol. June 2016;43:281-292. 14
4. Clark WF et al. The Chronic Kidney Disease Water Intake Trial: Protocol of a Randomized Controlled Trial. Can J Kidney Health Dis. 2017;4: 2054358117725106.
5. Chang Xu et al. Self-Fluid Management in Prevention of Kidney Stones: A PRISMA-Compliant Systematic Review and Dose-Response Meta-Analysis of Observational Studies. Medicine (Baltimore). 2015 Jul;94 (27): e1042.
6. Mitra P et al. Does the quality of drinking water matter in kidney stone disease. A study in West Bengal, India. Investig Clin Urol. 2018 May(3):158-165.
7. Post A et al. Creatine is a Conditionally Essential Nutrient in Chronic Kidney Disease: A Hypothesis and Narrative Literature Review. Nutrients. 2019 May 10:11(5).
8. Boero R et al. Salt intake and kidney disease. 2002 May-Jun:15(3):225-9.
9. Jhee, JH et al. Effects of Coffee Intake on Incident Chronic Kidney Disease: Community-Based Prospective Cohort Study. Am J Med. 2018. Vol 131 (12):1482-1490. December 2018.
10. Rybakowska IM et al. Effect of decaffeinated coffee on function and nucleotide metabolism in kidney. Mol. Cell Biochem. 2018 Feb:439(1-2):11-18.
11. Wijampreecha K et al. Association of coffee consumption and chronic kidney disease: A meta-analysis. Int J Clin Pract. 2017 Jan:71(1).
12. Shu X et al. Green tea intake and risk of incident of kidney stones: Prospective cohort studies in middle-aged and elderly Chinese individuals. Int J Urol. 2019 Feb: 26(2): 241-246.
13. Yi W et al. Green Tea Polyphenols Ameliorate the Early Renal Damage Induced by a High-Fat Diet via Ketogenesis/SIRT3 Pathway. Oxid Med Cell Longev. 2017: 9032792.
14. Naziroglu M et al. Apple cider vinegar modulates serum lipid profile, erythrocyte, kidney, and liver membrane oxidative stress in ovariectomized mice fed high cholesterol. J Membr Biol. 2014 Aug: 247(8):667-73.
15. Prezioso D et al. Dietary treatment of urinary risk factors for renal stone formation. A review of CLU Working Group. Arch Ital Urol Androl. 2015 Jul 7;87(2):105-120.
16. Liakopoulos V et al. Antioxidant Supplementation in Renal Replacement Therapy Patients: Is There Evidence? Oxid Med Cell Longev. 2019 Jan 15;20199109473. Ecollection 2019.
17. Khatami PG et al. The effects of high-dose vitamin E supplementation on biomarkers of kidney injury, inflammation, and oxidative stress in patients with diabetic nephropathy: A randomized, double-blind, placebo-controlled trial. J Clin Lipidol. 2016 Jul-Aug:10(4): 922-929. 15
18. Mune M et al. Vitamin E supplementation improves high density lipoprotein and endothelial functions in end-stage kidney disease patients undergoing hemodialysis. Clin Nephrol. 2018 Sep:90(3):212-221.
19. Shevchuk SV et al. The relationship between homocysteine level and vitamins B12, B9 and B6 in patients with chronic kidney disease. Wiad Lek. 2019;72(4):532-538.
20. Gerster H. No contribution of ascorbic acid to renal calcium oxalate stones. Ann Nutr Metab. 1997;41(5):269-282.
21. Malihi Z et a. Hypercalcemia, hypercalciuria, and kidney stones in long-term studies of vitamin D supplementation: a systematic review and meta-analysis. Am J Clin Nutr. 2016 Oct; 104(4):1039-1051.
22. Massy ZA et al. Magnesium-based interventions for normal kidney function and chronic kidney disease. Magnes Res. 2016 Apr 1:29(4):126-140.
23. Xu Y et al. Efficacy of coenzyme Q10 in patients with chronic kidney disease: protocol for a systematic review. BMJ Open. 2019 May 14:9(5); e029053.
24. Bakhshayeshkaram M et al. The Effects of Coenzyme Q10 Supplementation on Metabolic Profiles of Patients with Chronic Kidney Disease: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Curr Pharm Des. 2018;24 (31):3710-3723.
25. Ki Y et al. Effect of Coenzyme Q10 on Radiation Nephropathy in Rats. J Korean Med Sci. 2017 May;32(5):757-763.
26. Ustuner MA et al. Effects of benfotiamine and coenzyme Q10 on kidney damage induce gentamicin. Tissue Cell. 2017 Dec;49(6):691-696.
27. Kitada M and Kova D. Renal Protective Effects of Resveratrol. Oxid Med Cel Longev. 2013: 568093. Published online 2013 Nov 28.
28. Shimizu MH et al. N-acetylcysteine protects against renal injury following bilateral ureteral obstruction. Nephrol Dial Transplant. 2008 Oct 23(10):3067-74.
29. Wang AG et al. Effect of Acetyl-L-carnitine Used for Protection of Neonatal Hypoxic-Ischemic Brain Injury in Male and Female Rats. Neurochem Res. 2019 Apr 30.
30. Gholipur-Shahraki T et al. Effects of Carnitine on Nutritional Parameters in Patients with Chronic Kidney Disease: An Updated Systematic Review and Meta-Analysis. J Res Pharm Pract. 2018 Apr-Jun;7(2):57-68.
31. Zhang J and McCullough PA. Lipoic Acid in the Prevention of Acute Kidney Injury. Nephron. 2016: 134(3):133-140. 16
32. Z Li et al. Melatonin therapy protects against renal injury before and after release of bilateral ureteral obstruction in rats. Life Sci. 2019 Jul 15: 229:104-115.
33. Kumas M et al. Investigation of dose-dependent effects of berberine against renal ischemia/reperfusion injury in experimental diabetic rats. Nefrologia. 2019 Jul-Aug:39(4).
34. Qin X et al. Berberine Protects Glomerular Podocytes via Inhibiting Drp1-Mediated Mitochondrial Fission and Dysfunction. Theranostics. 2019 Feb 28:9(6): 1698-1713.
35. Gholampour F and Keikha S. Berberine protects the liver and kidney against functional disorders and histological damages induced by ferrous sulfate. Iran J Basic Med Sci. 2018 May: 21(5):476-482.
36. Ren YL et ak, Research progress of berberine in the treatment of diabetic kidney disease. Zhongguo Zhong Yao Za Zhi. 2017 Feb;42(3):438-442.
37. Lin Y et al. Berberine protects renal tubular cells against hypoxia/reoxygenation injury view the Sirt1/p53 pathway. J Nat Med. 2018 Jun;72(3):715-723.
38. Zhang X et al. Protective effect of berberine on high glucose and hypoxia-induced apoptosis via the modulation of HIF-1a in renbal tubular epithelial cells. Am J Transl Res. 2019 Feb 15;11(2):669-682.
39. Sen Z et al. Total Coumarins from Hydrangea paniculata against Cisplatin-Induced Acute Kidney Damage in Mice by Suppressing Renal Inflammation and Apoptosis. Evid Based Complement Alternat Med. 2017;2017:5350161.
40. Zhang S et al. Total Coumarins from Hydrangea paniculata Show Renal Protective Effects in Lipopolysaccharide –Induced Acute Kidney Injury via Anti-inflammatory and Antioxidant Activities. Front Pharmacol. 2017 Dec 14;8:872.
41. Sen Z et al. Coumarin glycosides from Hydrangea paniculata slow down the progression of diabetic nephropathy by targeting Nrf2 oxidation and smad 2/3-mediated profibrosis. Phytomedicine. 2019 Apr;57:385-395.
42. Li Y et al. Activation of Sirtuin 3 by Silibin Attentuates Mitochondrial Dysfunction in CIsplatin-induced Acute Kidney Injury. Front Pharmacol. 2017 Apr 5;8:178.
43. De Souza Santos V et al. Silymarin protects against radiocontrast induced nephropathy in mice. Life Sci. 2019 Jul 1;228:305-315.
44. Wei X et al. Activation of TRPV4 by dietary apigenin antagonizes renal fibrosis in deoxycorticosterone acetate (DOCA)-salt-induced hypertension. Clin Sci (Lond). 2017 Apr 1;131(7):567-581. 17
45. Sarchar S et al. Antiadhesive hyrdoalcoholic extract from Apium graveolens fruits prevents bladder and kidney infection against uropathogenic E. coli. Fitoterapia. 2018 Jun;127:237-244.
46. Zhong Y et al. Protective effects of apigenin against 3-MCPD-induce renal injury in rat. Chem Biol Interact. 2018 Dec 25;296:9-17.
47. Liu X et al. Huangqi-Danshen Decoction Ameliorates Adenine-Induced Chronic Kidney Disease by Modulating Mitochondrial Dynamics. Evid Based Complement Alternat Med. 2019 Jan 1: 2019.9574045.
48. He L et al. Effects of water extract of salvia miltiorrhiza against renal injury in rats exposed to cadmium. Zhonghua Yi Xue Za Zhi. 2017 Jan 3:97(1):57-61.
49. Xiang X et al. Salvia miltiorrhiza protects against diabetic nephropathy through metabolome regulation and wnt/B-catenin and TGY-B signaling inhibition. Pharmacol Res. 2019 Jan:139:26-40.
50. Zhang HF et al. Salvianolic acid A attenuates kidney injury and inflammation by inhibiting NF-kB and p38 MAPK signaling pathways in 5/6 nephrectomized rats. Acta Pharmacol Sin. 2018 Dec:39(12);1855-1864.
51. Kreydiyyeh SI and Usta J. Diuretic effect and mechanism of action of parlsey. J Ethnopharmacol. 2002 Mar;79(3):353-7.
52. Saeidi J et al. Therapeutic effects of aqueous extracts of Petroselinum sativum on ethylene glycol-induced kidney calculi in rats. Urol J. 2012 Winter;9 (1):361-6.
53. Atlas S et al. Protective effect of Diyarbakir watermelon juice on carbon tetrachloride-induced toxicity in rats. Food Chem Toxicol. 2011 Sep;49 (9):2433-8.
54. Chan KY et al. Excessive watermelon consumption causing hyperkalaemia and increased symptom burden of an end stage renal disease patient. Nephrology (Carlton). 2016 Aug;21(8):721.
55. Siddiqui WA et al. Evaluation of anti-urolithiatic and diuretic activities of watermelon (Citrullus lanatus) using in vivo and in vitro experiments. Biomed Pharmacother. 2018 Jan; 97-1212-1221.
56. Di Cerbo A et al. A nutraceutical diet based on Lespedeza spp., Vaccinium macrocarpon and Taraxacum officinale improves spontaneous feline kidney disease. Physiol Rep. 2008 Jun:6(12) e13737.
57. Yousefi-Ghale Salimi et al. Inhibitory effects of taraxasterol and aqueous extract of Taraxacum officinale on calcium oxalate crystallization: in vitro study. Ren Fail. 2018 Nov; 49(1):298-305. 18
58. Sanae M and Yasuo A. Green asparagus (Asparagus officinalis) prevented hypertension by an inhibitory effect on angiotension-converting enzyme activity in the kidney of spontaneously hypertensive rats. J Agric Food Chem. 2013 Jun 12;61(23):5520-5.
59. Poormoosavi SM et al. Protective effects of Asparagus officinalis extract against Bisphenol A-induced toxicity in Wistar rats. Toxicol Rep. 2018 Mar 9;5:427-433.
60. Ardakani Movaghati MR et al. Efficacy of black seed (Nigella sativa) on kidney stone dissolution. A randomized double-blind, placebo-controlled trial. Phytother Res. 2019 May;33(5):1404-1412.
61. Foroqui Z et al. Protective effect of Nigella sativa oil on cisplatin induced nephrotoxicity and oxidative damage in rate kidney. Biomed Pharmacother. 2017 Jan;85:7-15.
62. Huang KC et al. Chinese Herbal Medicine Improves the Long-Term Survival Rate of Patients With Chronic Kidney Disease in Taiwan: A Nationwide Retrospective Population-Based Cohort Study. Front Pharmacol. 2018 Oct 1:9:1117.
63. Ali BH et al. Effects of aqueous extract and anthocyanins of calyces of Hibiscus sabdariffa (Malvaceae) in rates with adeinin-induced chronic kidney disease. J Pharm Pharmacol. 2017 Sep;69(9):1219-1229.
64. Melzig MF. Goldenrod—a classical exponent of urological phytotherapy. Wein Med Wochenschr. 2004 Nov;154 (21-22):523-7.
65. Weir MA et al. Micro-Particle Curcumin for the Treatment of Chronic Kidney Disease-: Study Protocol for a Multicenter Clinical Trial. Can J Kidney Health Dis. 2018 Dec 5;5: 2054358118813088.
66. 52. Kang DG et al. Butein ameliorates renal concentration ability in cisplatin-induced acute renal failure in rats. Biol Pharm Bull. 2004 Mar:27(3):336-70.
67. Brown AC. Kidney toxicity related to herbs and dietary supplements: Online table of case reports. Part 3 of 5 series. Food Chem Toxicol. 2017 Sep;107(Pt A):502-519.
68. Luciano RL and Perazella MA. Aristolochic acid nepthropathy: epidemiology, clinical presentation, and treatment. Drug Saf. 2015 Jan 38(1):55-64.
69. Fernando-Prado R. Nutrients Turned into Toxins: Microbiota Modulation of Nutrient Properties in Chronic Kidney Disease. Nutrients. 2017 May 12;9(5).